Residency
Pharmacy Residency Programs (Hershey)
Penn State Health Milton S. Hershey Medical Center hosts a PGY-1 pharmacy residency and three PGY-2 pharmacy residencies in critical care, oncology and pediatrics.
On This Page
Our Residency Programs:
PGY-1 Pharmacy Residency
Established in 1985, the PGY-1 Pharmacy Residency is a rigorous one-year program designed to advance the training of pharmacists in all aspects of health-system pharmacy practice. With a strong emphasis on evidence-based pharmacotherapy, the program equips residents with the skills and experience needed to provide high-quality patient care in a complex healthcare environment. Six residents each year benefit from tailored learning experiences that foster individual interests and career goals.
PGY-2 Critical Care Pharmacy Residency
Established in 2017, this program offers two positions per year and focuses on providing advanced training in the management of critically ill patients across various intensive care units.
PGY-2 Oncology Pharmacy Residency (Candidate Status)
Launched in 2023, this one-resident-per-year program offers focused training in the care of oncology and hematology patients, preparing pharmacists to work as integral members of oncology care teams.
PGY-2 Pediatric Pharmacy Residency (Candidate Status)
Also introduced in 2023, this program offers one position annually and focuses on specialized pharmacotherapeutic care for neonatal and pediatric populations in both inpatient and ambulatory settings.

Your Residency. Our Commitment.
Penn State Health offers a dynamic and comprehensive pharmacy residency experience within an academic medical center environment that supports over 1,700 multidisciplinary trainees. Our residency programs are designed to prepare pharmacists for clinical excellence, leadership, and advanced practice in a wide range of healthcare settings.
Learn More about the Residency
Pharmacy residents in both the postgraduate year one (PGY-1) program and postgraduate year two (PGY-2) program are immersed in patient care pharmacotherapy opportunities consisting of several different practice areas.
Penn State Health Milton S. Hershey Medical Center is a large, tertiary care acute adult teaching hospital.
Penn State Health Children’s Hospital features the region’s highest level neonatal and pediatric intensive care units including a Level I trauma center. Penn State Health Children’s Heart Group offers comprehensive congenital heart care including surgery as well as support with ECMO.
Penn State Cancer Institute promotes multidisciplinary approaches to cancer care.
Each year, the emergency department provides services for more than 75,000 visits. Nearly 30,000 patients are admitted to the hospital, and 1 million outpatient clinic visits occur.
Pharmacy residents at Penn State Health are immersed in a supportive and academically rich environment. Our Department of Pharmacy, staffed by over 200 dedicated professionals, delivers comprehensive, patient-centered medication management across a diverse health system. Key highlights include:
Interdisciplinary Learning
Pharmacists are embedded in unit-based teams across medicine, surgery, cardiology, pediatrics, and other specialties, working side-by-side with physicians, nurses, and other healthcare providers.
Advanced Pharmacy Services
The department features decentralized pediatric and adult pharmacy services, outpatient clinics, emergency services with 24/7 pharmacist presence, investigational drug services, and outpatient pharmacy locations.
Clinical Integration
Our team of more than two dozen clinical pharmacists and specialists provides services such as therapeutic drug monitoring, disease state management, medication reconciliation, and discharge counseling—all with a strong emphasis on patient-facing care.
Education and Precepting
Each year, pharmacy preceptors oversee over 85 pharmacy student rotations, contributing to a culture of teaching and continuous professional development.
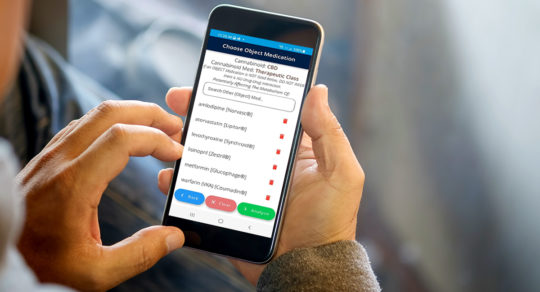
Technology-Driven Practice
Residents benefit from a state-of-the-art automated drug distribution and medication management system, supporting efficient and safe medication use.
General Application Information
Interested applicants must register with the American Society of Health-System Pharmacists (ASHP) Residency Matching Program and apply through the Pharmacy Online Residency Centralized Application Service (PhORCAS).
To be considered for the Pharmacy Residency, a PhORCAS application and online application must be completed by early January. Exact deadline each year can be found on the ASHP Residency Directory.
Applicants must submit all of the following through PhORCAS:
PGY-1 candidates:
A letter of interest, including a statement on diversity, equity and inclusion
Copy of curriculum vitae
Official copy of college transcript
Three (3) letters of recommendation
PGY-2 candidates:
Letter of intent addressing the following:
Interests and reasons for pursuing advanced training
Strengths and areas for improvement
Career goals for the next 5 years
Copy of curriculum vitae
Official, finalized copy of college transcript (including degree(s) conferred)
Three (3) letters of recommendation
Application Review
Each residency program reviews all complete applications submitted by the deadline. Selected candidates will be contacted directly to schedule an interview.
Interview Invitations
Interviews are offered by invitation only and are typically held from mid-January through February. Invitations will be sent via email, and prompt responses are appreciated.
Interview Format
The PGY-1 program generally interviews up to four candidates per day, while tailoring the schedule to provide a personalized experience. A portion of the day is conducted in a group format (including a program overview, presentation, and lunch with current residents), but most interview components are individualized. Interviews may be conducted in person or virtually, depending on availability and candidate preference.
Interview days typically begin between 8:00 and 9:00 a.m. and conclude by 3:00 p.m. Activities include:
Interviews with the Residency Program Director and preceptors
Lunch and tour with current residents (in-person interviews)
Break and separate resident session (virtual interviews)
Pharmacotherapy competency assessment
“About Me” slide presentation prepared by each candidate to help preceptors get to know you
Questions?
For questions about the application or interview process, please contact the appropriate Program Director.
PGY-1 Curriculum
Pharmacy residents at Hershey Medical Center engage in a wide variety of educational, clinical, and professional development experiences designed to support the growth of clinical pharmacists prepared for advanced practice in diverse settings.
Participation in patient case presentations and topic discussions.
24/7 clinical on-call (in-house from 7 a.m. - 9 p.m.)
After orientation, residents serve as first-call clinical consultants approximately once per week (7 a.m. – 9 p.m. in-house; from home overnight), with an assigned clinical preceptor available as second-call.
The on-call program includes responding to adult code blue alerts and participating in ACLS response while on-site.
Residents are the first point of contact for positive blood cultures with organisms carrying resistance genes (e.g., ESBL, CRE, MRSA, VRE). Using a protocol-driven algorithm, residents may order the first dose of an active antimicrobial agent when appropriate.
Consults for a wide variety of drug information questions, occasional pharmacokinetic consults, and evaluation of non-formulary requests are examples of other activities completed while on-call.
Hospital pharmacy staffing
Residents staff every third weekend (Saturday and Sunday, 8-hour shifts), including one on-call day per weekend.
One weekday evening shift is scheduled every three weeks.
Four additional 8-hour shifts are required during the residency year.
Staffing is primarily in the central pharmacy or IV room alongside technician and pharmacist colleagues.
Longitudinal Ambulatory Clinics
Anticoagulation Clinic: Assigned half-day each week for two-thirds of the year at a nearby outpatient location. Residents provide point-of-care management in direct patient care visits.
Elective Clinics: One half-day per week for one-third of the year in an elective setting, such as:
Primary Care Clinic (Cocoa Avenue)
Rheumatology Clinic (Middletown)
Oncology Specialty Pharmacy (Hershey Medical Center)
Pulmonology Specialty Pharmacy
Additional options may be available based on interest and preceptor availability.
Research and Scholarly Activities
Minor Project or Medication Use Evaluation: Each resident completes an minor project during the first half of the year and presents findings at a national residency showcase, typically just prior to the ASHP Midyear Clinical Meeting.
Major Project: Residents develop an IRB-approved project with preceptor mentorship, build a data collection tool, and complete analysis. Projects are presented at an annual Pharmacy Residency Conference.
Pharmacy and Therapeutics Committee
Residents will serve as secretary for at least two meetings (System P&T or Formulary) during the program year.
Each resident will complete at least two deliverables in the form of class review, monograph, guideline, protocol, utilization management criteria or orderset.
Teaching and Precepting Opportunities
Lecture to the Penn State College of Medicine Physician Assistant Program on a pharmacotherapy topic (early in the year).
Provide an ACPE-accredited continuing education session to the pharmacy department (January–March).
Precept pharmacy students during clinical rotations.
Facilitate journal clubs for residents and students.
Optional teaching certificate through Shenandoah University.
Each of the following learning experiences have a minimum of one rotation each:
Critical Care (Medical ICU, Surgical/Anesthesia ICU, or Heart & Vascular ICU)
Medicine (Adult Internal Medicine or Family and Community Medicine Service)
Advanced Adult Medicine or Advanced Pediatric Medicine
General Pediatrics (if the resident is a previous pediatric APPE, the possibility exists to substitute NICU, PICU or pediatric hematology/oncology)
Infectious Diseases
Pharmacy Administration & Leadership
Each of the following required experiences or training areas continues throughout the program.
Ambulatory Care
Oncology Specialty Pharmacy
Primary Care Clinic
Pulmonology Specialty Pharmacy
Rheumatology Clinic
Ambulatory Care Anticoag Clinic (two-thirds of the year)
Pharmacy & Therapeutics
Hospital Pharmacy Practice
Major Project
Medication Safety
Minor Project
Teaching, Education, and Dissemination of Knowledge
A number of electives are available in the Pharmacy Residency, including:
Adult Bone Marrow Transplant
Adult Hematology/Oncology
Advanced Pediatric Medicine
Antimicrobial Stewardship
Cardiology
Emergency Medicine
Family and Community Medicine
HVICU
Immunocompromised Infectious Diseases
Inpatient Psychiatry
Investigational Drug Service
Medical Intensive Care Unit
Neonatal Intensive Care
Neuroscience Critical Care (NCCU)
Pediatric Hematology/Oncology
Pediatric ICU
Specialty Pharmacy
Surgical/Anesthesia Intensive Care Unit
PGY-2 Curriculums
Required rotations:
Emergency Medicine
Heart and Vascular Intensive Care Unit
ICU Float
Medical Intensive Care Unit
Medical Intensive Care Unit II
Neurocritical Care Unit
Pediatric Intensive Care Unit
Surgical Intensive Care - Anesthesia
Surgical Intensive Care - Trauma
Surgical Intensive Care - Advanced Anesthesia & Trauma
Elective rotations:
Adult Hematology/Oncology
Heart and Vascular Intensive Care Unit II
Infectious Disease
Medical Intensive Care Unit III
Neonatal Intensive Care Unit
Neurocritical Care Unit II
Longitudinal Rotations:
Education
Hospital Pharmacy Practice
Major Project
Medication Safety
Medication Use Evaluation
Required rotations:
Adult Hematology
Adult Stem Cell Transplant/Cellular
Inpatient Oncology/Transitions of Care
Oncology Practice Management
Oncology/Investigational Drug Service
Oncology/Sterile Products
Outpatient Oncology
Pediatric Hematology/Oncology
Specialty Oncology
Elective rotations:
Immunocompromised Infectious Diseases
MICU/Critical Care Oncology
Pain/Palliative Care
Pediatric Hematology/Oncology - II
Longitudinal Rotations:
ACPE/Fellow Lectures
Drug Use Policy
Hospital Pharmacy Practice
Medication Safety
MUE/Research Project
Oncology P&T Subcommittee
Core rotations:
General Pediatrics
General Pediatrics II (focus on teaching)
Neonatal Intensive Care
Pediatric Hematology/Oncology
Pediatric Infectious Diseases/Antimicrobial Stewardship
Pediatric Intensive Care
Elective rotations:
Medication Safety
Neonatal Intensive Care II
Pediatric Emergency medicine
Pediatric Hematology/Oncology II
Pediatric Intensive Care II
Pediatric Palliative Care/Hummingbird
Pediatric Specialty Services (Pulmonology, Cardiology, Nephrology, Neurology)
Longitudinal rotations:
ACPE Presentation/PA Lecture
Clinical On-Call Component (Code response)
Hospital Pharmacy Practice
Medication Safety
Pediatric P&T Subcommittee
Project/Research
Teaching Certificate (optional)
Contact and Leadership

PGY-1 Pharmacy Residency Program Director, Pharmacy Residency (Hershey, Pa.)

Director of Pharmacy, Clinical Services, Pharmacy Administrations, Pharmacy Residency (Hershey, Pa.)

PGY-2 Oncology Program Director, Pharmacy Residency (Hershey, Pa.)

PGY-2 Pediatrics Program Director, Pharmacy Residency (Hershey, Pa.)